Audiological Management II
In the grand sense, the terms audiological (re)habilitation and aural (re)habilitation refer to a wide range of modalities employed by the audiologist to maximize the hearing-impaired patient’s ability to live and communicate in a world of sound. Many clinicians use the term rehabilitation when working with someone who has an impairment of an already-developed skill, such as an adult with an adventitious hearing loss, and habilitation when dealing with an individual who has not yet developed a skill, such as a child with prelingual hearing loss. The modalities of audiological intervention include the use of physical instruments such as hearing aids, cochlear implants, tactile aids, and hearing assistance technologies, as well as therapeutic approaches like patient and family counseling, developing effective communication strategies, and auditory-visual training. To this list must be added referrals to and interactions with other professionals who are involved with the patient’s management, such as speech-language pathologists, physicians, psychologists, teachers, etc.
We will cover audiological management in two chapters. This chapter will deal with basic concepts and principles pertaining to hearing aids per se. Our coverage of audiological management will continue in the next chapter, beginning with the clinical use of hearing aids and other instruments, and then moving one to cochlear implants, hearing assistance technology, and intervention approaches.
 Hearing Aids
Hearing Aids
It almost goes without saying that the first order of business in the audiological management of a hearing-impaired person must be to increase the intensities of sounds so they become audible. Hearing aids are devices that boost sound levels so the patient can hear them. This process is called amplification.
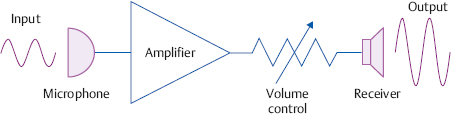
Most simply, a hearing aid amplifies sounds just like a megaphone, except the amplified sound is directed right into the listener’s ear. It is easiest to think of a hearing aid in terms of its major parts, as shown in Fig. 15.1. The hearing aid’s microphone picks up sounds and converts them into an electrical signal. A device that transforms energy from one form to another is called a transducer. Thus, the microphone is an acoustic-to-electrical transducer. Once the sound has been changed into an electrical signal it can be manipulated by electronic circuits. Obviously, the principal manipulation is to boost its intensity, that is, to amplify it. This is done by the amplifier. The amplified electrical signal is then converted back into sound by an electrical-to-acoustic transducer or loudspeaker. The hearing aid’s loudspeaker is called the receiver. The amplified sound from the receiver is directed into the patient’s ear. Two other components of all hearing aids should be mentioned at this time. One is the battery, which provides the power to accomplish all of the hearing aid’s functions. The other is the earmold, which is the object actually inserted into the patient’s ear. In fact, the majority of modern hearing aids are completely contained within the earmold itself. Earmolds are almost always custom-made from an impression taken of the ear.
The sounds picked up by the microphone are called the input to the hearing aid and the sounds produced by the receiver are called the output. The patient hears the output from the hearing aid. The amount of amplification is called gain. Suppose the input is speech at 60 dB SPL and the output is the same speech signal that has been amplified to 95 dB SPL. How much amplification has occurred? The obvious answer is 35 dB because the signal coming out of the instrument is 35 dB higher than the signal that went in. Thus, gain is simply the difference in decibels between the intensity coming out of a hearing aid and the intensity that went in. Numerically, gain (in dB) equals output (in dB SPL) minus input (in dB SPL). Ten decibels of gain means the output is 10 dB higher than the input, and 0 dB of gain means the input and output are the same. Notice that input and output are given in SPL, but gain is not expressed in SPL. The reason is that the input and output are physical magnitudes, whereas gain refers to the difference between them. In fact, 10 dB of gain is simply referred to as “10 dB gain.” (The quantitatively oriented student should note that gain is actually the ratio of the intensity of the output to the intensity of the input.) Any hearing aid has a range of gains that it can generate, and the patient has some degree of control over this gain by using a volume control (more technically called a gain control), just like the volume control of a radio.
Fig. 15.1 A simplified hearing aid diagram showing the microphone, amplifier, and receiver. Notice how the output from the receiver is larger than the input into the microphone. The battery is not shown for simplicity.
The sound level of a hearing aid’s output cannot be limitless. The greatest sound magnitude that can be produced by a hearing aid is quite descriptively called its maximum power output (MPO) or output sound pressure level (OSPL). We will see later that OSPL is more completely called OSPL90, which means how much is coming out of the hearing aid (“O”) in decibels of sound pressure level (“SPL”) when the input to the hearing aid is a 90 dB SPL signal (“90”). For example, an OSPL of 124 dB means that 124 dB SPL is the strongest sound the hearing aid is capable of producing. In other words, OSPL refers to the output of the hearing aid in dB SPL when the hearing aid is saturated. In fact, OSPL used to be called saturation sound pressure level (SSPL).
To understand what we mean by OSPL, suppose you set a hearing aid to its highest gain by turning its volume control all the way up and you also keep increasing the input. The output will get bigger and bigger as the input rises, but the output will eventually reach a maximum. Here, the output cannot get any higher no matter how much you raise the input (remember that the volume control is already turned all the way up). At this point we say the hearing aid is saturated, or that saturation has occurred. This is analogous to what happens when you keep pouring more and more water into a sponge. It will soak up all the water until some maximum amount is absorbed. At that point we say that the sponge is saturated, meaning that it cannot hold any more water no matter how much more water you pour into it. Similarly, once the hearing aid’s maximum power output is reached, its output cannot become any greater than this ceiling no matter how much more the input might increase or the volume control might be turned up. When this happens, the parts of the amplified sound that would have exceeded the ceiling are clipped off, resulting in a distortion of the amplified signal descriptively known as peak clipping.
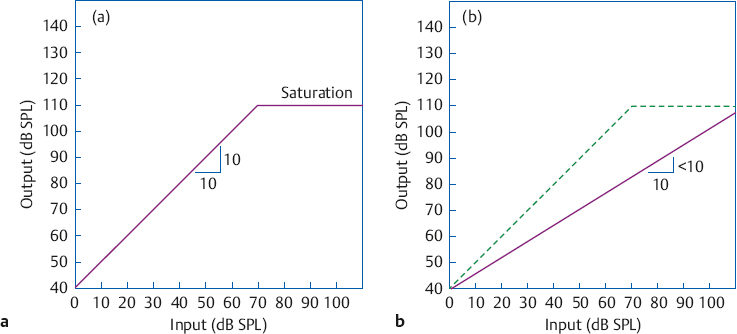
These notions are illustrated by the input-output (I-O) function in Fig. 15.2a. The diagonal line shows how output increases with input up to a maximum value, where the line becomes horizontal because output no longer rises with increasing input. The diagonal line represents linear amplification, and shows that each 10 dB increase of input (on the x-axis) results in a 10 dB increase in the output (on the y-axis). This one-for-one relationship continues until saturation is reached, where output no longer increases with input. In this example, the I-O function becomes flat (saturates) when the output is 110 dB SPL. Parts of the output that would have been above this 110 dB saturation level would be clipped off.
Many hearing aids have automatic gain control (AGC) circuits that are usually employed to “slow down” the rate of amplification for louder sounds. Automatic gain control means that output from the hearing aid is changed automatically when the input changes. Compression is a kind of AGC where a certain increase in input results in a smaller increase the output increase, as shown by the solid line in Fig. 15.2b. Here we see that a 10 dB increase in the input level results in less than a 10 dB increase in the output level. Notice how compression amplification causes the I-O curve to be shallower than it would have been with linear amplification (shown by the dashed line for comparison). As a result, peak clipping is avoided. In addition, compression is used to prevent outputs from becoming strong enough to be uncomfortably loud, which is often desirable for patients who have trouble with loudness recruitment. The amount of compression is expressed by a compression ratio, which is simply the relationship of input level changes to output level changes. A compression ratio of 2:1 means that every 2 dB input increase results in an output increase of only 1 dB. Since every 1 dB input increase results in 1 dB output increase with linear amplification, it has a compression ratio of 1:1.
The student should also be aware of a process called expansion, although its applications are beyond the introductory level. Expansion means that the output level rises faster than the input level, so that a 10 dB increase of the input results in more than a 10 dB increase in the output. In this case, the I-O curve is steeper than it would have been with linear amplification. Analogous to the compression ratio, an expansion ratio of 1:2 means that every 1 dB input increase results in an output increase of 2 dB.
Two more commonly encountered hearing aid components are worthy of mention. One of these is the tone control. It adds flexibility to the instrument by adjusting the relative levels of the higher and lower frequencies much like the bass and treble on a stereo set.
The telecoil is a circuit that allows the hearing aid to pick up magnetic signals generated by many telephone receivers instead of using the microphone. Telecoils are associated with a switch labeled “M/T” or “M/T/MT,” allowing the patient to select between using the hearing aid’s microphone (M) in the normal manner, using the telecoil (T) while bypassing the microphone, or in some cases using the microphone and telecoil simultaneously (MT). The telecoil allows the patient to hear the telephone signal without interference from noises in the room, and/or to attend to a telephone conversation that would not be possible using the microphone. The MT position might be selected when the patient desires to hear the phone clearly but also needs to hear what is going on around her, or when she needs her hearing aid to monitor her own voice while speaking on the phone.
Types of Hearing Aids
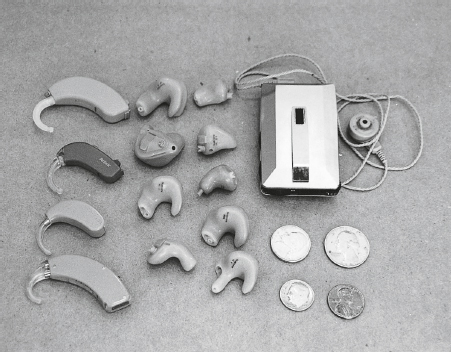
Hearing aids are most broadly classified in terms of whether they are body or ear-level devices, and among the latter, whether they are worn behind the ear, in the ear, or built into eyeglass frames. Fig. 15.3 shows several examples. Originally, the larger body aids were the most common devices, but smaller and less conspicuous devices now dominate the market (e.g., Strom 2000). One is tempted to conclude that this simply reflects the ability of technological advances to meet patients’ desires for hearing aids that are cosmetically acceptable. While the cosmetic issue is real and highly relevant, it is by no means the only reason for the preponderance of small instruments. Technological advances have not only made it possible for modern hearing aids to be smaller, but more importantly modern hearing aids are capable of being genuine high-fidelity devices (Killion 1993). In addition, having a device in the patient’s ear means the microphone is picking up sounds as they appear at the patient’s ear. This permits the listener to receive a more realistic representation of his acoustic environment, and maximizes the ability to take advantage of binaural cues.
Body Hearing Aids
Body hearing aids contain all of their components and controls (except for the receiver and earmold) in a case about the size of a small pocket calculator. A wire leads from the case to the receiver and earmold at the patient’s ear. The case is usually worn somewhere on the chest. Typical locations are in a chest-level pocket; clipped to a shirt, jacket, or undergarment; or in a specially made harness. Body instruments now account for less than 1% of the hearing aids dispensed in the United States.
Body instruments have always been the most powerful hearing aids, and this continues to be true. Thus, body aids are primarily used for the most severe hearing losses. However, considerable amounts of gain are also available in modern ear-level instruments, so high power is no longer the exclusive domain of the body instrument. Because of their size, body aids have controls and batteries that are larger, more accessible, and easier to manipulate than other types of hearing instruments. This is advantageous for patients with arthritis and other handicapping conditions, as well as for some elderly patients and younger children. An unfortunate dilemma exists because economic considerations make it practical for body aids to be manufactured only as powerful (high-gain) instruments. This is a problem for individuals who need large controls due to manual dexterity or other limitations, as well as low to moderate amounts of gain.
In addition to being big enough to accommodate larger components and batteries, another reason body aids can provide the greatest amounts of gain involves the problem of acoustic feedback. This is the whistle or whine produced when the output from the receiver is picked up by the microphone; feedback is a bigger problem when the microphone and receiver are closer together than when they are farther apart. The wide separation between the microphone (on the chest) and receiver (at the ear) with body aids makes feedback less of a problem than it is for ear-level instruments, where the two transducers are very close together.
Body instruments have many limitations, as well. The most obvious problem is cosmetic undesirability, but it is not the only one. Many of the problems are due to the location of the microphone on the torso instead of at ear level. Noise is picked up by the microphone when clothing brushes across the case. The amount and thickness of clothing covering the case can reduce the sound reaching the microphone. (Consider how different one’s aided hearing would be with the microphone covered by a sweater and overcoat.) The body itself can adversely affect the intensity and spectrum of the sounds reaching the microphone. These effects are known as the “body shadow” and the “body baffle.” Finally, body aids cause sounds to be picked up as though the ears were located on the chest instead of on the sides of the head. This distorts the perception of auditory space and detracts from the perceptual advantages afforded by binaural hearing even if two hearing aids are being used.
Ear-Level Hearing Aids
Ear-level instruments have all of their components in a small package worn in or near the ear, and comprise almost all hearing aids now being dispensed in the United States. They include behind-the-ear, in-the-ear, in-the-canal, and eyeglass instruments. A hearing aid is an ear-level instrument as long as the microphone and receiver are at the patient’s ear. This includes currently available or future ear-level units that use a radio signal (or wire) to communicate with signal processing circuits contained in a case that might be kept in one’s shirt pocket. In general, the smaller ear-level instruments provide less gain and flexibility than the larger ones, but there is extensive overlap among instrument types. Moreover, the ongoing development of programmable and signal processing hearing aids (see below) continues to cloud the traditional distinctions. Feedback has been limiting factor for ear-level devices, although feedback cancellation technology is available in digital hearing aids (see, e.g., Ross 2006; Johnson, Ricketts, & Hornsby 2007).
Behind-the-ear (BTE) or post-auricular instruments have their components contained in a crescent-shaped plastic case that fits behind the auricle. The amplified sound produced by the receiver, which is located in the case of the instrument, is transmitted via a plastic tube to an earmold in the patient’s ear. The receiver-in-the-canal (RIC) hearing aid is a noteworthy modification of the BTE arrangement in which the receiver is located inside of the patient’s ear canal, and is connected to the body of the instrument by a tiny wire. The more powerful models of BTE instruments rival the amounts of gain that could only be provided by body aids in the past, although many patients with very severe and profound losses still require body instruments.
Behind-the-ear hearing aids are preferred for pediatric patients because earmolds must be replaced frequently as infants and children grow, and also because they can be easily coupled with assistive listening devices (AAA 2013; see Chapter 16).
Over the years, BTEs were supplanted by in-theear instruments (described below), accounting for slightly less than 20% of the hearing aids dispensed in the United States in 1999. However, the advent of mini– or micro– BTE hearing aids (of which the RIC is one type) came with a dramatic reversal of the earlier trend, so that BTEs now account for ~ 51% of all instruments dispensed (Kirkwood 2007).
Eyeglass hearing aids have their components built into the temple piece of the patient’s glasses. Similar to BTEs, the receiver output goes through a plastic tube to an earmold in the patient’s ear. These instruments have various practical problems because they are part of and inseparable from the patient’s eyeglasses, and are rarely used anymore.
In-the-ear (ITE) hearing aids have all of their components built into the earmold. In spite of their small size, the technology has progressed to the point that a majority of patients can now be fitted with ITE-type instruments. In-the-ear hearing aids vary widely in size. The largest ones fill the whole concha and extend into the ear canal. Smaller units take up less and less of the concha, and the smallest ones fit completely into the ear canal. The latter group constitutes a category of instruments called completely-in-the-canal (CIC) hearing aids. To be considered a CIC instrument, the outermost part of the device must be at least 1 to 2 mm inside of the ear canal entrance. Very tiny CIC instruments are sometimes called invisible in-the-canal (IIC) hearing aids. Most CICs also are deep canal fittings, meaning that the device extends into the bony part of the canal so its receiver end is within ~ 5 mm of the eardrum. (Actually, a deep canal fitting can be achieved with any kind of hearing aid as long as its earmold extends this deep into the external auditory meatus.) The various types of ITE instruments collectively account for ~ 49% of the hearing aids dispensed in the United States (Kirkwood 2007).
In addition to their obvious cosmetic advantage, CIC and IIC hearing aids also offer several acoustic benefits (e.g., Chasin 1994; Gudmundsen 1994; Mueller 1994). For example: (1) locating the microphone inside the meatus entrance makes it possible to take advantage of pinna and concha effects; (2) compared with shallower ones, deep canal fittings provide more gain and output because the sound is directed into a smaller volume; and (3) they are less likely to make the wearer’s own speech sound as if he is talking inside a barrel because the occlusion effect is minimized in the bony section of the canal. On the other hand, deep canal fittings also have some potential for negative outcomes (e.g., Branda 2012; Leavitt, Welch, & Thompson 2013). For example, there is the possibility of abrasions of the ear canal and injuries to the eardrum and middle ear structures (especially when deep earmold impressions are being made), as well as the possibility that the enhanced sound amplitudes might cause progression of hearing loss.
Directional Hearing Aids
Hearing aids with directional microphones are called directional hearing aids (e.g., Ricketts & Mueller 1999; Valente 2000; Ricketts & Dittberner 2002; Ricketts 2005). Directional microphones are designed to be more sensitive to sounds coming from certain directions and less sensitive to sounds coming from other directions. This is in contrast to the more common type of microphone, which is more or less equally sensitive to sounds coming from all directions, or omnidirectional. In the directional mode, the hearing aid provides more amplification for sounds coming from the front compared with sounds coming from behind the patient. As a result, directional hearing aids provide the patient with an improved signal-to-noise ratio (SNR) in situations where the desired signal is coming from the front and noise is coming mainly from behind. Most patients experience directional benefits; and small albeit significant directional advantages have been found even for patients with severe hearing losses, at least under difficult listening conditions (e.g., Ricketts & Hornsby 2006).
The benefits afforded by directional amplification depend on various factors, such as listening situations. For example, Walden, Surr, Cord, and Dyrlund (2004) found that hearing aid users appear to prefer the directional mode in situations with noisy backgrounds when the signal comes from a nearby source in front of them, but prefer the omnidirectional setting in quiet environments as well as in noisy situations when the signal source is farther away. In addition, the speaker is not always in front of the listener. For example, instruments capable of favoring locations next to or behind the listener have been shown to be useful when speaking to others in a car (e.g., Wu, Stangl, Bentler, & Stanziola 2013). Directional amplification on a full-time basis is also problematic for children because it reduces their ability to attend to environmental signals and overhear conversations coming from all around them, as well as opportunities for incidental learning (AAA 2013).1 Thus, patients should be advised to switch between the directional and omnidirectional settings depending on the listening situation, rather than arbitrarily keeping the hearing aid in the directional mode at all times. Signal processing technologies that provide the hearing aid with adaptive directional functions are also available (e.g., Ricketts & Henry 2002; Kuk, Keenan, Lau, & Ludvigsen 2005).
Signal Processing Hearing Aids
Digital hearing aids now account for over 90% of the instruments dispensed in the United States (Kirkwood 2007). In contrast to traditional hearing aids that use standard (analog) electronic circuits to amplify and otherwise adjust the signal, digital or digital signal processing (DSP) hearing aids use an analog-to-digital (A/D) converter to transform the signal entering the microphone into digital form (i.e., a code in which binary numbers represent the sound signal). The instrument then accomplishes all aspects of the amplification process digitally (analogous to how a personal computer handles the activities involved in word processing or computer games). After digital processing, the signal is transformed back into analog form by a digital-to-analog (D/A) converter, and is then transduced into amplified sound by a receiver. Digital hearing aids provide a host of signal processing and adaptive functions (in which the hearing aid automatically reacts or adapts to the nature of the signal), such as sophisticated compression schemes, feedback suppression, noise reduction, switching between directional and omnidirectional modes, and programmable amplification, among others.
1 Ching, O’Brien, Dillon, et al (2009) suggested it is probably not necessary to be concerned about a child’s ability to hear safety-related and warning signals coming from behind because (1) it is unlikely that the directional hearing aid would reduce the sound coming from behind enough for this to occur, and (2) part of the decrease likely would be counteracted by the hearing aid’s compression circuit.
Programmable Hearing Aids
Programmable hearing aids are instruments that can be programmed to provide several different kinds of amplification characteristics for use under different kinds of circumstances, such as speech communication in quiet and in the presence of competing noises, listening to music, etc. The wearer can select among the different settings using a switch on the hearing aid itself or with a small remote control device that can be kept in a pocket or handbag.
Bone-conduction Hearing Aids
The hearing aids described so far have been air-conduction instruments in which the sound is directed into the ear from a miniature loudspeaker (the receiver) via the normal air-conduction route. Bone-conduction hearing aids present amplified sound to the patient using a bone-conduction vibrator just like the ones used for bone-conduction audiometry (Chapter 5). The vibrator is typically held in place with a spring headband or built into the temple portion of eyeglasses. Bone-conduction instruments are used only when air-conduction hearing aids are ruled out because of atresia of the ear canal or certain conductive pathologies like active drainage from the ear, or in situations in which ear disease is activated when an earmold is used.
Surgically Implantable and Bone-Anchored Hearing Aids
Surgically implantable hearing aids may be warranted in some patients who have permanent conductive hearing losses, particularly if they cannot use regular hearing aids because of medical considerations such as those mentioned for bone-conduction instruments. Implantable middle ear devices typically attach to the ossicular chain (e.g., Goebel et al 2002; Miller & Sammeth 2002; Spindel 2002; Franz 2007; Traynor & Fredrickson 2007; Bassim & Fayad 2010).
In contrast to the surgically implanted devices, the BAHA bone-anchored hearing aid (Fig. 15.4) uses an external bone-conduction device that attaches to a titanium screw implanted in the side of the skull in a manner analogous to dental implants (e.g., Spitzer, Ghossaini, & Wazen 2002; Wazen, Spitzer, Ghossaini, et al 2003; Bosman, Snik, Mylanus, & Cremers 2006, 2009; Pfiffner, Caversaccio, & Kompis 2011; Colquitt, Loveman, Baguley, et al 2011; Janssen, Hong, Chadha 2012; Bosman, Snik, Hol, & Mylanus 2013). The BAHA instrument can be worn with a headband (Softband; Fig. 15.4c) by children too young for implantation, others who cannot have the surgery, and during testing and trial periods by patients who are candidates for the device. Bone-anchored instruments offer several advantages over conventional bone-conduction hearing aids, such as the elimination of feedback, headband pressure, and the instability of vibrator positioning, as well as some improvement in high-frequency response and reduced distortion. The BAHA is also useful as an approach to CROS amplification (see below) in cases of single-sided deafness by picking up sounds on the deaf side and transmitting them to the hearing side via bone-conduction (e.g. Hol et al 2010; Snapp, Fabry, Telischi, Arheart, & Angeli 2010; Wazen et al 2010; Desmet, Bouzegta, Hofkens, et al 2012; Pai, Kelleher, Nunn, et al 2012).

Comments
Post a Comment